GLAUCOMA FAQs
What is Glaucoma?
Can Glaucoma be treated?
How is Intraocular Pressure (IOP) involved?
What are the Risk Factors For Developing Glaucoma?
Do All People With High IOP Get Glaucoma?
Why Is Corneal Thickness Relevant?
Do Patients With Glaucoma Always Have High IOP?
Is Treatment Different For Normal Tension Glaucoma?
What Kind Of Glaucoma Do I Have?
What Should I Expect When I Attend the Glaucoma Clinic?
SURGICAL OPTIONS
Trabeculectomy
Tube/Shunt
Non-Penetrating
OTHER PROCEDURES
New Procedures
Revision Procedures
WHAT IS GLAUCOMA?
The term 'glaucoma' refers to a group of conditions that may cause irreversible vision loss through damage to the optic nerve.
In glaucoma, nerve tissue is lost from the optic nerve (the nerve carrying visual signals from the eye to the brain). As it builds up over time, this damage can cause progressive, irreversible damage to vision.
CAN GLAUCOMA BE TREATED?
Yes - Glaucoma can be treated using a number of methods but it is important to pick up glaucoma early, before there is major vision loss. If glaucoma is treated, the damage to vision can be stabilised to stop it getting worse. The damage is irreversible – in other words vision lost from glaucoma cannot be restored once it has been lost. In patients with advanced disease or at high risk of losing vision, it is important to treat early and aggressively.
How is Glaucoma Treated?
HOW IS INTRAOCULAR PRESSURE INVOLVED (IOP)
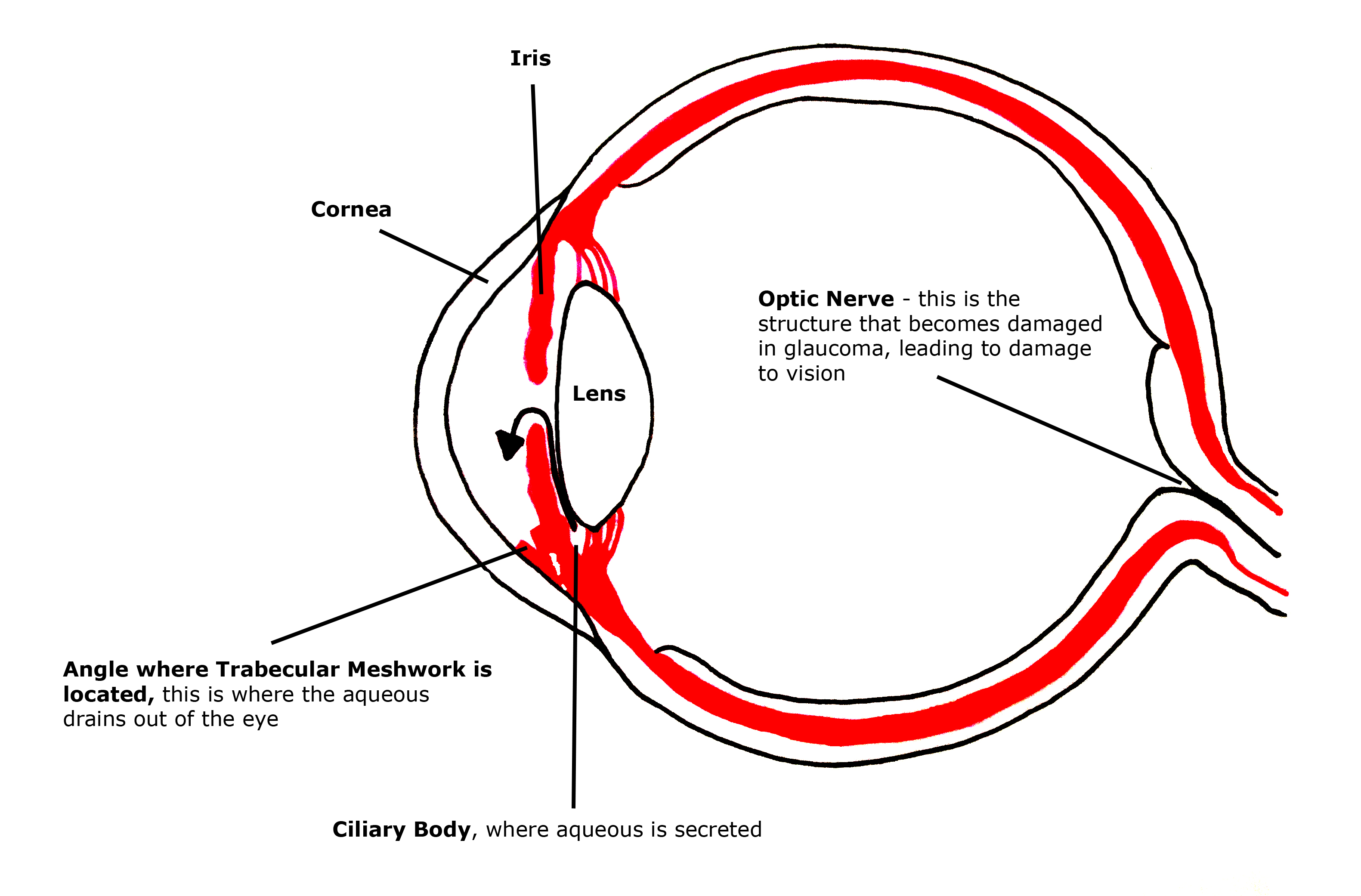
All our eyes contain a clear fluid called aqueous. Aqueous provides oxygen and nutrients to many of the different tissues at the front of the eye. The aqueous also helps to maintain the eyeball's tension, thereby keeping its shape. The aqueous is produced by a structure inside the eye called the ciliary body. Aqueous leaves the eyeball through a structure called the trabecular meshwork. This is located in the angle formed by the clear cornea and the coloured iris. Aqueous drains via the trabecular meshwork into a canal around the eye called the canal of Schlemm and then into the bloodstream.
The pressure in the eye (IOP) depends on the balance of the production of aqueous (inflow) and of aqueous leaving the eye (outflow). Any disorder that leads to a blockage or reduction in outflow can lead to elevated IOP.
Elevated IOP is one of the main risk factors for developing glaucoma. The normal range of IOP is 10 – 21 mmHg. All current treatments for glaucoma involve lowering the IOP.
WHAT ARE THE RISK FACTORS FOR DEVELOPING GLAUCOMA?
• High IOP
• Ageing
• Family history of glaucoma, particularly if first degree relatives (parents, siblings, offspring)
• Myopia (short sightedness) for open angle
• Hypermetropia (long sightedness) for closed angle
• Certain Ethnic Groups
DO ALL PEOPLE WITH HIGH IOP GET GLAUCOMA?
Ocular hypertension is a condition where the IOP is consistently over 21 mmHg but there is no other evidence of glaucoma. In other words, although the IOP is high, the optic disc shows no features of glaucoma and there is no glaucoma related vision damage in the visual field test.
People with ocular hypertension are at increased risk of developing glaucoma and this risk will increase according to the presence of other risk factors:
• Positive family history of glaucoma (having a parent or sibling with glaucoma)
• 'Suspicious' optic disc appearance
• Thin central corneal thickness
• IOP greater than 30 mmHg
WHY IS CORNEAL THICKNESS RELEVANT?
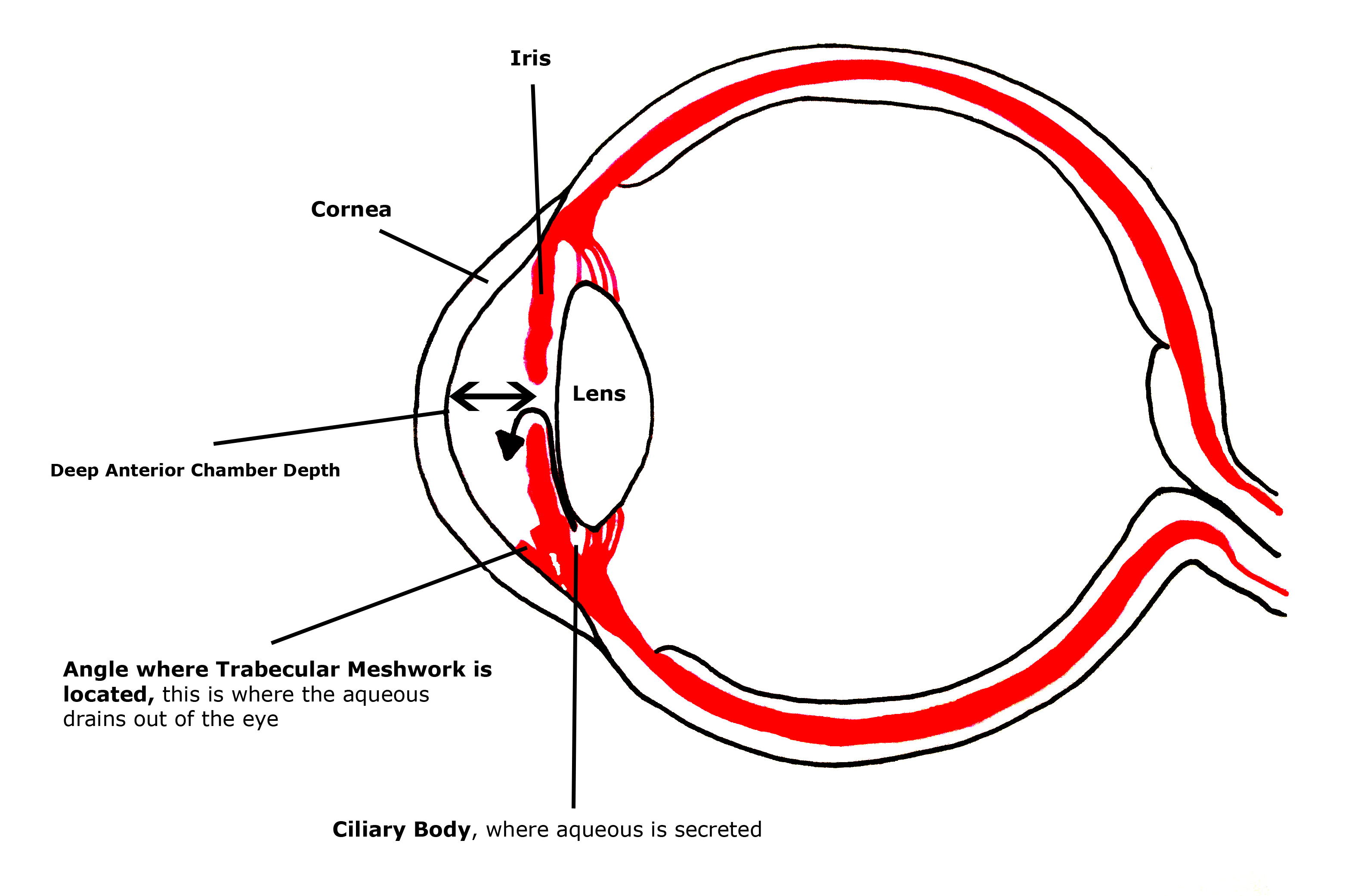
The corneal thickness is usually measured at the first clinic visit using an ultrasound device. IOP measurements may be read too high if the thickness is above average or too low if the thickness is below average.
Patients with thinner than average thickness corneas (less than 500 microns) may be at increased risk of glaucoma, depending on other risk factors. A thick cornea (greater then 570 microns) may indicate that risk of glaucoma may be low, in the absence of other risk factors.
DO PATIENTS WITH GLAUCOMA ALWAYS HAVE HIGH IOP?
Up to 40% of people with glaucoma never have a high IOP reading (usually called normal tension glaucoma). This is, in fact, the most common presentation of glaucoma in people of Japanese or Korean origin. Normal tension glaucoma is usually considered a variant on the spectrum of primary open angle glaucoma.
Certain other risk factors may be associated with the development of normal tension glaucoma:
• History of migraine
• History of Raynaud's Phenomenon (cold hands and feet)
• History of significant blood loss
• Very low blood pressure during sleep or when lying flat
All of these risk factors are assumed to be related to a predisposition to reduced blood flow to the optic nerve, which may contribute (along with IOP) to the development of glaucoma in people with normal tension glaucoma.
IS TREATMENT DIFFERENT FOR NORMAL TENSION GLAUCOMA?
The only method we currently have of treating glaucoma is to lower the IOP.
This is regardless of the type of glaucoma, and whether the IOP measurements are high or within normal limits.
It is hoped that 'neuroprotective' treatments, which have been used successfully to treat other neurodegenerative disorders such as Parkinson's Disease and Alzheimer's Disease, will be useful in preserving vision in glaucoma, particularly normal tension glaucoma. At the time of writing, there is no convincing evidence supporting the use of neuroprotective agents but studies are still ongoing.
WHAT KIND OF GLAUCOMA DO I HAVE?
Glaucoma is usually divided into open angle and closed angle forms.
To understand about the angle and its relevance to IOP click here
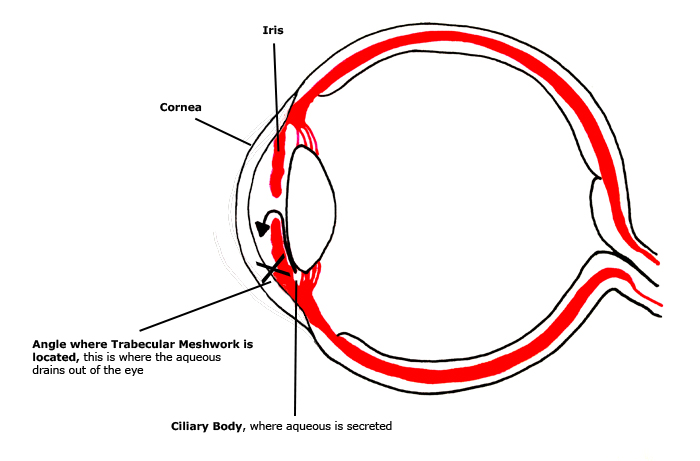
If the angle is narrow, or closed (in other words the edge of the iris touches the edge of the cornea), then it is difficult for the aqueous to leave the eye, so IOP will go up.
When the angle is closed, patients are described as having angle closure, whether or not the pressure is high. If the angle is closed and there are features of glaucoma damage in the optic nerve then the patient has angle closure glaucoma.
Open Angle
Most glaucoma cases in the UK have an open angle. In these cases it is assumed that the high pressure is caused by problems in the trabecular meshwork that cannot be seen with the naked eye.
Primary and Secondary Glaucomas
Glaucoma is further divided into primary and secondary forms.
Secondary
Secondary means that the high pressure or angle closure is caused by some other medical factor. There are secondary open angle problems and secondary angle closure problems.
Common causes of secondary glaucoma include:
• High IOP after vitreo-retinal surgery
• High IOP after corneal surgery
• High IOP following the use of steroids
• High IOP following uveitis (inflammation) in the eye
With secondary glaucomas, the underlying cause will need to be treated, as well as the high IOP. Often the treatment for secondary glaucomas is surgical as the pressures can be very high and sight may be threatened over a short space of time. For further information regarding secondary glaucomas, click here
Primary
Primary means that there is no identifiable underlying cause for the glaucoma or of the high pressure. In the UK, the most common cause of glaucoma is primary open angle glaucoma.
There are two relatively common risk factors for developing glaucoma with an open angle. These are called pigment dispersion syndrome and pseudoexfoliation. These risk factors are common enough that they are often classed together with primary open angle (called chronic open angle glaucoma in the NICE guidance).
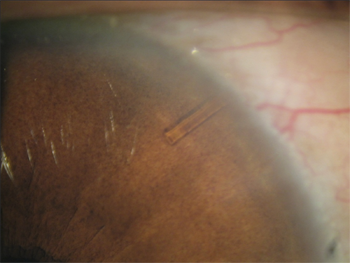
Pigment dispersion syndrome (PDS)
PDS occurs when pigment from the back of the iris is shed and the granules of pigment block the trabecular meshwork, causing the IOP to go up.
In some patients, the pressure can go extremely high particularly after periods of intense exercise when pigment shedding is increased.
When the high IOP causes glaucomatous optic nerve damage, it is called pigmentary glaucoma.
PDS is more common in men in their 30-40s with myopia (short-sightedness).
Occasionally, pigment dispersion can occur as a secondary complication from cataract surgery.
Pseudoexfoliation (PXF)
PXF is caused by a type of fibrillar material that is deposited throughout the eye (and indeed the rest of the body), in particular on the surface of the lens.
PXF material is shed from the lens and this can 'clog up' and damage the trabecular meshwork, increasing the IOP leading to glaucoma.
When there is glaucomatous optic nerve damage, it is called pseudoexfoliative glaucoma.
PXF occurs in all races, but is perhaps more common in Scandinavian and Southern Mediterranean races.
The treatment of ocular hypertension and glaucoma due to pseudoexfoliation or pigment dispersion is the same as for other forms of ocular hypertension and glaucoma.
TREATMENT
MEDICAL
Most patients who are diagnosed with glaucoma, or considered to be at sufficiently high risk of developing glaucoma, will be offered treatment with an IOP-lowering eye drop.
Eye drops for glaucoma need to be taken every day and are life-time treatments unless told otherwise by your doctor.
If the first eye drop does not work, or the IOP-lowering effect is not sufficient it may be substituted for another drop or another drop added.
There are 5 different classes of IOP-lowering drops for glaucoma but generally speaking if three or more drops are required to stabilise the condition then other treatment options should be considered. Each eye drop can cause side effects and often patients will discontinue an individual drop because they have developed intolerance.
Other ways to treat Glaucoma:
LASER TREATMENT
Laser Peripheral Iridotomy (LPI) For Angle Closure
LPI is a form of laser used to reverse angle closure. The laser is administered at the slit lamp under topical anaesthetic. The procedure involves making a small hole in the iris, covered by the upper eyelid. This allows aqueous to pass from the back to the front of the iris and vice versa, thereby deepening the angle.
LPI is usually offered as first line treatment in people who have primary angle closure and primary angle closure glaucoma. Some patients with primary angle closure may present acutely with a very high IOP. LPI is required as part of the treatment in these eyes, along with drops to lower the IOP and drops that open up the angle.
LPI may cause inflammation, bleeding and elevated IOP but these effects are usually transient and can be treated with a short course of topical treatment. Serious complications such as visual disturbance are extremely rare.
LPI is not a suitable treatment for most secondary forms of angle closure as the hole will eventually close up, causing the IOP to go up again. In these cases, if an iridotomy is considered then it should be done surgically (a surgical iridectomy).
A more definitive treatment, which can be considered if iridotomy has not opened the angle sufficiently or if the patient already has significant cataract, is to perform lens extraction surgery with insertion of an intraocular lens. This has the effect of completely and definitively widening the angle. Please refer to the section on cataract surgery for more information.
Some patients with primary angle closure and primary angle closure glaucoma will effectively be treated just with peripheral iridotomy or lens extraction. Some may require eye drops to lower the IOP. Occasionally, patients may require further intervention (surgery or other forms of laser) if the glaucoma continues to worsen despite the aforementioned treatments.
Selective laser trabeculoplasty (SLT)
SLT is a laser treatment, delivered at the slit lamp (not in the operating theatre), which can be used to treat POAG and ocular hypertension.
During the treatment, laser energy acts on the trabecular meshwork, stimulating better aqueous drainage, thereby lowering IOP.
SLT is a useful treatment, because it is relatively simple and has a low risk of complication. The main risks are slight pain, inflammation, and failure. In some patients it can work for a prolonged period, in some cases giving to up to 5 years of IOP control without drops.
It is perhaps most effective at the earliest stages of the disease when POAG or ocular hypertension are first picked up. It can also be used as an alternative to drops or to try to reduce the number of the drops later on in the disease process, although success is more limited.
Cyclodiode
Cyclodiode is a procedure in which laser is applied on the surface of the white of the eye and this leads to a reduction of aqueous production by the ciliary body.
This can be a very effective method for lowering IOP but it needs to be done in the operating theatre with a local anaesthetic injection to prevent discomfort.
Cyclodiode may cause inflammation leading to a reduction in vision in some patients. It has therefore usually been reserved for refractory cases (in other words cases where all other treatments have failed) or blind painful eyes with high IOP. Increasingly now it is being used successfully in certain circumstances to treat high IOP in eyes with good vision.
Endocyclophotocoagulation (ECP)
ECP is a variation of cyclodiode treatment, whereby an endoscopic camera probe is introduced into the eye through a small wound and this allows a laser to be fired directly onto the parts of the ciliary body where aqueous is produced.
ECP is particularly useful as it can be combined with cataract surgery and so is therefore useful for lowering IOP in glaucoma patients undergoing cataract surgery.
Other ways to treat Glaucoma:
WHEN SHOULD SURGERY BE CONSIDERED?
Generally speaking, surgery should be offered in any of the following circumstances:

1) Patient is losing vision (visual field is getting worse) despite maximal topical medication (3+ different topical medications)
2) Patient has very high IOP despite drops and is at significant risk of losing vision
3) Patient presents with advanced disease
4) Patient is intolerant of multiple drops or is having difficulties taking treatment
5) Patient chooses to have surgery rather than other forms of treatment
In some cases, patients will be put on a pressure-lowering tablet (acetazolamide – Diamox), whilst they are waiting for surgery. This tablet is very effective at lowering IOP but in most cases it should not be used long term because of side effects, including kidney damage and kidney stones.
Other ways to treat Glaucoma:
TRABECULECTOMY
Trabeculectomy is a highly effective surgical treatment for glaucoma, which when successful can stabilise the condition and get patients off drops. An advantage of trabeculectomy over other treatments is that it can achieve low target IOPs, so can be used effectively in normal tension glaucoma.
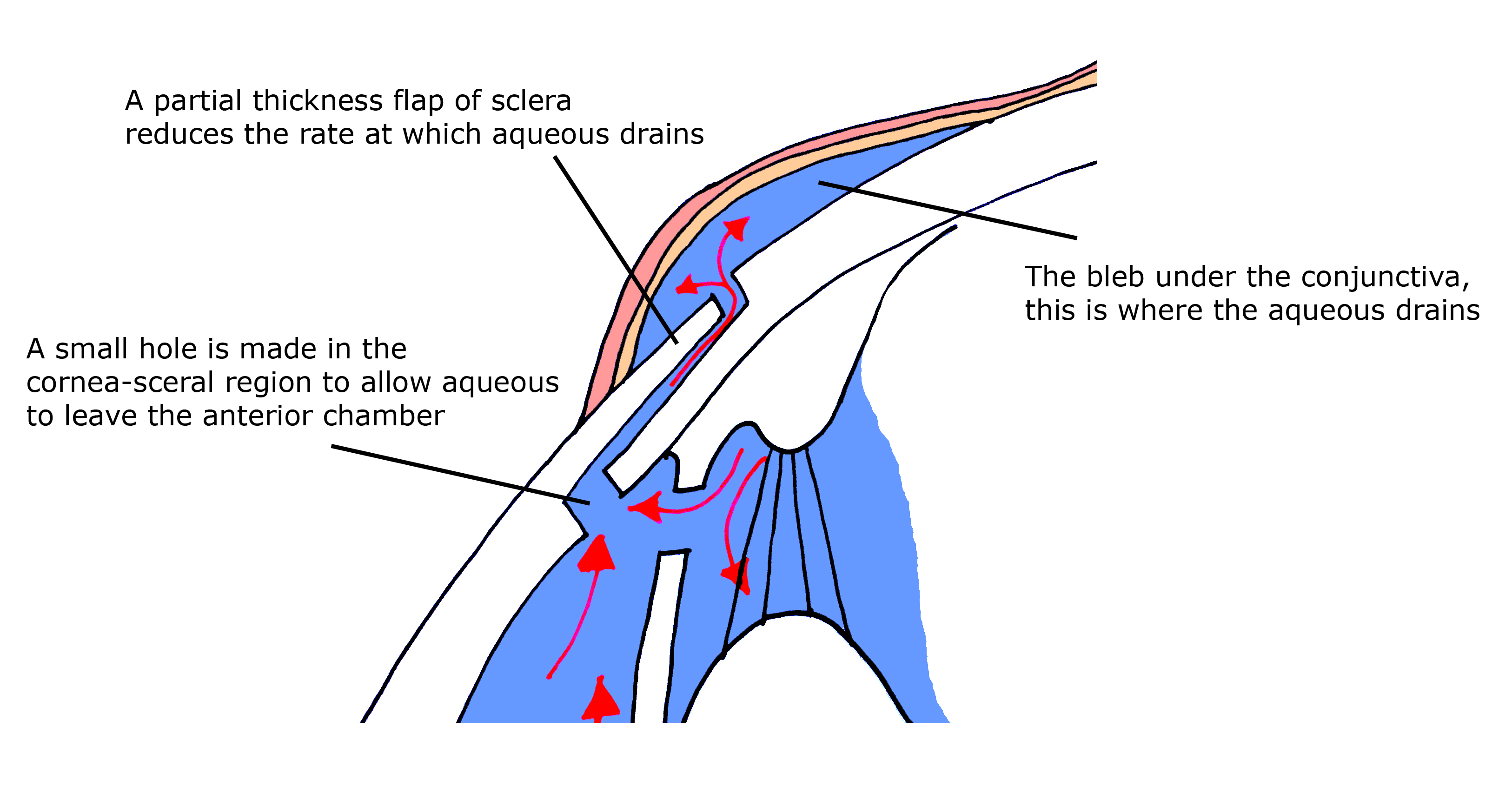
Trabeculectomy works by allowing aqueous to drain out of the eye into a 'bleb' at the top of the eye, covered by the upper lid. It is usually undertaken as day case surgery under local anaesthetic but can also be done with the addition of sedation or general anaesthetic. If successful, trabeculectomy will lead to a stabilisation of glaucoma for a number of years without requiring any IOP-lowering drops.
The main reason trabeculectomies stop working or fail is due to scarring of the tissues around the bleb. At the time of surgery, drugs such as mitomycin C or 5 fluorouracil may be used to reduce the long-term risk of scarring. Post-operatively, trabeculectomies require close monitoring and topical anti-inflammatory drops (steroids) usually for the first 12 weeks after the surgery to ensure that failure is prevented. Serious complications of trabeculectomy are rare but include infection or bleeding that may lead to vision loss in less than 1 in 1000 cases.
TUBES/SHUNTS
Implantation of a glaucoma drainage device (GDD - also known as a tube or aqueous shunt) works by diverting aqueous from the front of the eye via a tube to a drainage plate stitched onto the white of the eye, much further back than where a trabeculectomy trap door is stitched.
It is felt that less scarring occurs further back in the eye, so tubes may give better long-term success in eyes where trabeculectomies have already failed.
Tubes are a useful option when a trabeculectomy with mitomycin has failed and needling to resurrect the trabeculectomy has been unsuccessful. Tubes are usually considered as the first choice surgical procedures in eyes in which there are is a high risk of trabeculectomy failure or at increased risk of hypotony (low pressure complications) with trabeculectomy surgery. In these eyes tube surgery may be highly successful and safer than trabeculectomy surgery.
NON-PENETRATING SURGERY
There is a variant of glaucoma surgery called 'non-penetrating surgery' which can be considered for the same indications as trabeculectomy.
Advocates of this technique believe that it carries less risk than trabeculectomy because it may be less likely to cause hypotony or infection. Recent studies of modern trabeculectomy techniques (Kirwan, et al. Ophthalmology 2013) have, however, shown that these risks are very rare in skilled hands.
The argument against non-penetrating surgery is that it may not achieve the same low target pressures as trabeculectomy so may not be suitable in cases where the glaucoma is deteriorating despite relatively low IOP.
A new variation of non-penetrating surgery whereby part of the surgical dissection is carried out using a CO2 laser will be trialled at Moorfields Eye Hospital later in 2014, with Mr Strouthidis being one of the investigators.
WHAT ABOUT NEWER PROCEDURES?
What about newer procedures?
A number of newer procedures and devices have been introduced and these are usually all grouped together under the banner of 'minimally invasive glaucoma surgery' (MIGS).
The rationale for developing these techniques is to try to find quicker, simpler procedures that might be safer in terms of reduced risk of complication as compared to the conventional techniques of tubes or trabeculectomy. There has been a plethora of devices and techniques and they are divided as follows:
Scleral Bypass
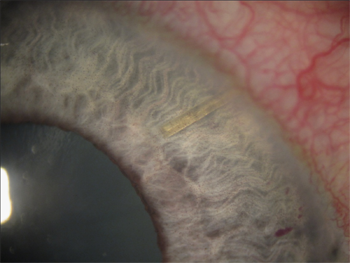
These divert aqueous from the anterior chamber into the sub-conjunctival space via the sclera. This is the same pathway as used by trabeculectomies and tubes.
The Xen Nano (pictured above) manufactured by Aquesys, is a micro-tube that utilises this technique. It is being used in a clinical trial undertaken at Moorfields, for which Mr Strouthidis is the principal investigator.
Canal Bypass
Schlemm's canal is the canal around the circumference of the front of the eye into which aqueous drains from the trabecular meshwork.
In the outer wall of schlemm's there are a series of aqueous collector channels that take the aqueous out of the eye via the blood stream.
By reducing the resistance to flow within Schlemm's canal, it is expected that there will be increased drainage into the collector channels.
The iStent device manufactured by Glaukos is a microstent that is implanted through the trabecular meshwork into schlemm's canal.
The Hydrus implant manufactured by Ivantis is a stent that enters schlemm's canal via the trabecular meshwork but spans a distance of the canal as a form of scaffold, thereby increasing flow and access to the aqueous channels.
Trabectome manufactured by Neomedix is a surgical procedure where diathermy (focused heat therapy) is used to cleanly remove the inner wall of schlemm's canal, thereby exposing the aqueous channels to the inner part of the eye – this device is available at Moorfields and the procedure is performed by Mr Strouthidis.
Suprachoroidal Bypass
The suprachoroidal space refers to a spongy layer in the eye between the sclera (the white of the eye) and the choroid (the inner blood vessel layer of the eye). It is a potentially unlimited space for the drainage of aqueous so has long been theorised as a possible surgical drainage site for glaucoma treatment.
A number of shunts have been developed with the intention of draining aqueous from the anterior chamber into the suprachoroidal space.
The Cypass microstent, manufactured by Transcend is currently being trialled within the UK and there is also a suprachoroidal shunt available from the manufacturers of the iStent.
Reducing Aqueous Production
Strictly speaking, techniques that reduce aqueous production are not technically MIGS procedures but are included as alternative, newer treatments.
ECP has been discussed here. ECP is available at Moorfields and the procedure is performed by Mr Strouthidis.
There is an alternative treatment to cyclodiode for refractory glaucoma called HIFU (high intensity focused ultrasound), which is an adaptation of a treatment for prostate cancer. Here rather than laser energy, ultrasound is used to reduce the production of aqueous by the ciliary body. Early results suggest that it is a less painful, quicker procedure than cyclodiode.
Where Do MIGS Procedures Fit Into Current Glaucoma Practice?
There is a lot of interest in these new procedures but at the time of writing there is no long-term evidence to suggest that they are as effective at stabilising glaucoma as trabeculectomy or tube surgery.
They are not yet a standard part of NHS glaucoma care and as yet their role in treatment has not been clearly defined. In nearly all cases, the target IOP achieved is not as low as trabeculectomy BUT the procedures have the advantage of being relatively simple, quick and safe.
Most experts believe that their role will be as an adjunct to cataract surgery in patients with glaucoma who are undergoing cataract surgery and in whom a reduction in topical IOP-lowering medications will be beneficial.
In order for the role of these newer surgical treatments to be better defined, clinical trials are needed to assess their effectiveness. Until then, one needs to maintain a degree of skepticism about their long-term effectiveness.
Many of these devices and treatments are, or will be, available at Moorfields (NHS) where they will be investigated as part of ongoing clinical trials. Some devices are already available for use in the private sector, but as stated previously, conventional techniques will usually be the preferred option.
REVISION SURGERY
What Is Revision Surgery?
Revision surgery is an umbrella term for any kind of surgical intervention that is used to try to get a tube or trabeculectomy to work again or to reverse any form of complication associated with glaucoma drainage surgery.
Trabeculectomy Revision
If trabeculectomy surgery fails, then it is possible to try to get it working again by 'needling' to cut away the scar tissue. Occasionally, it is possible to open up the previous trabeculectomy trap door to get it to start working again. Repeat or redo trabeculectomies are not, however, associated with a high long-term success rate so tube surgery is usually offered where a trabeculectomy followed by multiple needlings has failed.
Occasionally trabeculectomies may become uncomfortable, may leak aqueous (thereby increasing the chances of infection) or have chronically low pressures causing poor vision. In these cases, complex revision surgery (often requiring donor graft material) may be required to reverse the problem whilst still trying to maintain trabeculectomy function (ie long term IOP control).
Revision Of Tubes
Tube revision surgery is required if the tube erodes, requiring donor patching, or if the tube needs to be resited. Tubes which are overdraining (IOP too low) may need to be explored surgically and have a ligating suture added or a stent (such as supramid) inserted into the tube lumen.
Often eyes with tubes have had multiple surgeries making revision surgery difficult; surgery on these eyes requires a great deal of experience to prevent further complications and to ensure a good outcome.