GLAUCOMA FAQs
What is Glaucoma?
Can Glaucoma be treated?
How is Intraocular Pressure (IOP) involved?
What are the Risk Factors For Developing Glaucoma?
Do All People With High IOP Get Glaucoma?
Why Is Corneal Thickness Relevant?
Do Patients With Glaucoma Always Have High IOP?
Is Treatment Different For Normal Tension Glaucoma?
What Kind Of Glaucoma Do I Have?
What Should I Expect When I Attend the Glaucoma Clinic?
SURGICAL OPTIONS
Trabeculectomy
Tube/Shunt
Non-Penetrating
OTHER PROCEDURES
New Procedures
Revision Procedures
What about newer procedures?
A number of newer procedures and devices have been introduced and these are usually all grouped together under the banner of 'minimally invasive glaucoma surgery' (MIGS).
The rationale for developing these techniques is to try to find quicker, simpler procedures that might be safer in terms of reduced risk of complication as compared to the conventional techniques of tubes or trabeculectomy. There has been a plethora of devices and techniques and they are divided as follows:
Scleral Bypass
These divert aqueous from the anterior chamber into the sub-conjunctival space via the sclera. This is the same pathway as used by trabeculectomies and tubes.
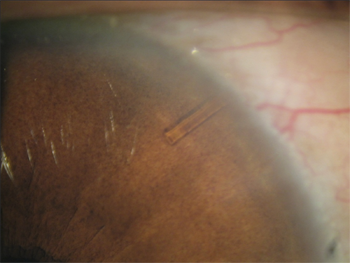
The Xen Nano (pictured above) manufactured by Aquesys, is a micro-tube that utilises this technique. It is being used in a clinical trial undertaken at Moorfields, for which Mr Strouthidis is the principal investigator.
Canal Bypass
Schlemm's canal is the canal around the circumference of the front of the eye into which aqueous drains from the trabecular meshwork.
In the outer wall of schlemm's there are a series of aqueous collector channels that take the aqueous out of the eye via the blood stream.
By reducing the resistance to flow within Schlemm's canal, it is expected that there will be increased drainage into the collector channels.
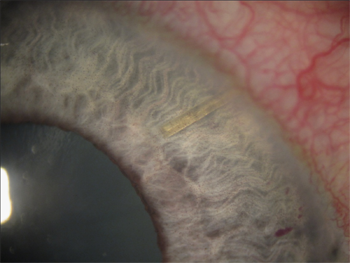
The iStent device manufactured by Glaukos is a microstent that is implanted through the trabecular meshwork into schlemm's canal.
The Hydrus implant manufactured by Ivantis is a stent that enters schlemm's canal via the trabecular meshwork but spans a distance of the canal as a form of scaffold, thereby increasing flow and access to the aqueous channels.
Trabectome manufactured by Neomedix is a surgical procedure where diathermy (focused heat therapy) is used to cleanly remove the inner wall of schlemm's canal, thereby exposing the aqueous channels to the inner part of the eye – this device is available at Moorfields and the procedure is performed by Mr Strouthidis.
Suprachoroidal Bypass
The suprachoroidal space refers to a spongy layer in the eye between the sclera (the white of the eye) and the choroid (the inner blood vessel layer of the eye). It is a potentially unlimited space for the drainage of aqueous so has long been theorised as a possible surgical drainage site for glaucoma treatment.
A number of shunts have been developed with the intention of draining aqueous from the anterior chamber into the suprachoroidal space.
The Cypass microstent, manufactured by Transcend is currently being trialled within the UK and there is also a suprachoroidal shunt available from the manufacturers of the iStent.
Reducing Aqueous Production
Strictly speaking, techniques that reduce aqueous production are not technically MIGS procedures but are included as alternative, newer treatments.
ECP has been discussed here. ECP is available at Moorfields and the procedure is performed by Mr Strouthidis.
There is an alternative treatment to cyclodiode for refractory glaucoma called HIFU (high intensity focused ultrasound), which is an adaptation of a treatment for prostate cancer. Here rather than laser energy, ultrasound is used to reduce the production of aqueous by the ciliary body. Early results suggest that it is a less painful, quicker procedure than cyclodiode.
Where Do MIGS Procedures Fit Into Current Glaucoma Practice?
There is a lot of interest in these new procedures but at the time of writing there is no long-term evidence to suggest that they are as effective at stabilising glaucoma as trabeculectomy or tube surgery.
They are not yet a standard part of NHS glaucoma care and as yet their role in treatment has not been clearly defined. In nearly all cases, the target IOP achieved is not as low as trabeculectomy BUT the procedures have the advantage of being relatively simple, quick and safe.
Most experts believe that their role will be as an adjunct to cataract surgery in patients with glaucoma who are undergoing cataract surgery and in whom a reduction in topical IOP-lowering medications will be beneficial.
In order for the role of these newer surgical treatments to be better defined, clinical trials are needed to assess their effectiveness. Until then, one needs to maintain a degree of skepticism about their long-term effectiveness.
Many of these devices and treatments are, or will be, available at Moorfields (NHS) where they will be investigated as part of ongoing clinical trials. Some devices are already available for use in the private sector, but as stated previously, conventional techniques will usually be the preferred option.