GLAUCOMA FAQs
What is Glaucoma?
Can Glaucoma be treated?
How is Intraocular Pressure (IOP) involved?
What are the Risk Factors For Developing Glaucoma?
Do All People With High IOP Get Glaucoma?
Why Is Corneal Thickness Relevant?
Do Patients With Glaucoma Always Have High IOP?
Is Treatment Different For Normal Tension Glaucoma?
What Kind Of Glaucoma Do I Have?
What Should I Expect When I Attend the Glaucoma Clinic?
SURGICAL OPTIONS
Trabeculectomy
Tube/Shunt
Non-Penetrating
OTHER PROCEDURES
New Procedures
Revision Procedures
TRABECULECTOMY
Trabeculectomy is a highly effective surgical treatment for glaucoma, which when successful can stabilise the condition and get patients off drops. An advantage of trabeculectomy over other treatments is that it can achieve low target IOPs, so can be used effectively in normal tension glaucoma.
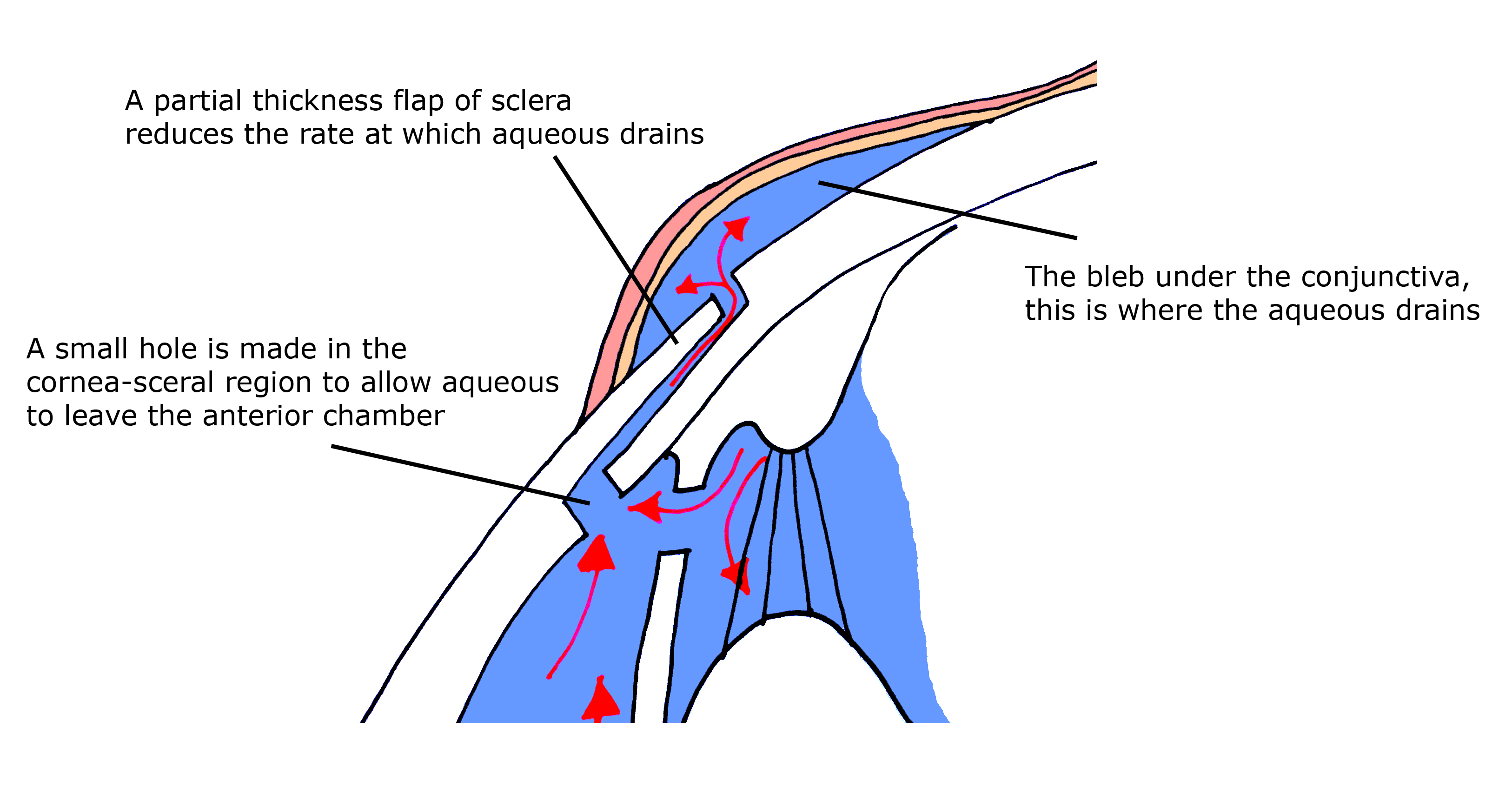
Trabeculectomy works by allowing aqueous to drain out of the eye into a 'bleb' at the top of the eye, covered by the upper lid. It is usually undertaken as day case surgery under local anaesthetic but can also be done with the addition of sedation or general anaesthetic. If successful, trabeculectomy will lead to a stabilisation of glaucoma for a number of years without requiring any IOP-lowering drops.
The main reason trabeculectomies stop working or fail is due to scarring of the tissues around the bleb. At the time of surgery, drugs such as mitomycin C or 5 fluorouracil may be used to reduce the long-term risk of scarring. Post-operatively, trabeculectomies require close monitoring and topical anti-inflammatory drops (steroids) usually for the first 12 weeks after the surgery to ensure that failure is prevented. Serious complications of trabeculectomy are rare but include infection or bleeding that may lead to vision loss in less than 1 in 1000 cases.